Ideas of Reference Psychosis in 2025: An Exploration of Evolving Concepts and Treatment Approaches
Related Articles: Ideas of Reference Psychosis in 2025: An Exploration of Evolving Concepts and Treatment Approaches
- 60th Birthday Celebrations For Women: A Guide To Unforgettable Memories In 2025
- Cheap Meal Ideas For 3 In 2025: Nourishing Meals On A Budget
- Gift Ideas For Women 2025: The Ultimate Guide To Impress Her
- Ideas Of Reference Delusions In 2025: An Exploration Of Current Trends And Future Implications
- Best Business Ideas To Make Money In 2025: A Comprehensive Guide To Future-Proof Your Income
Introduction
With enthusiasm, let’s navigate through the intriguing topic related to Ideas of Reference Psychosis in 2025: An Exploration of Evolving Concepts and Treatment Approaches. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
Video about Ideas of Reference Psychosis in 2025: An Exploration of Evolving Concepts and Treatment Approaches
Ideas of Reference Psychosis in 2025: An Exploration of Evolving Concepts and Treatment Approaches
Introduction
Ideas of reference (IOR) psychosis, a subtype of delusional disorder, is characterized by the persistent belief that seemingly unrelated events or objects have personal significance to the individual. In recent years, advancements in neuroscience and psychology have shed new light on the underlying mechanisms and treatment options for this condition. This article aims to provide an overview of the current understanding of IOR psychosis, explore emerging concepts, and discuss future directions in treatment.
Pathophysiology and Neurobiology
The pathophysiology of IOR psychosis remains complex and multifaceted. Neuroimaging studies have identified abnormalities in brain regions involved in self-referential processing, such as the medial prefrontal cortex and posterior superior temporal sulcus. These regions are responsible for integrating information about the self and the environment, and their dysfunction may lead to the misinterpretation of external stimuli as being personally relevant.
Additionally, dysregulation of neurotransmitter systems, particularly dopamine and serotonin, has been implicated in IOR psychosis. Dopamine hyperactivity may contribute to the heightened salience and significance attached to environmental cues, while serotonin dysfunction may impair cognitive flexibility and the ability to dismiss irrelevant information.
Clinical Presentation and Diagnosis
Individuals with IOR psychosis typically experience persistent beliefs that seemingly unrelated events or objects have personal significance to them. These beliefs can be positive or negative, and they often involve themes of persecution, grandeur, or reference to specific individuals or groups.
The diagnosis of IOR psychosis requires the presence of the following criteria:
- A persistent belief that seemingly unrelated events or objects have personal significance
- The belief is not culturally appropriate or consistent with the individual’s background
- The belief is not explained by another mental disorder, such as schizophrenia or a mood disorder
- The belief causes significant distress or impairment in functioning
Differential Diagnosis
IOR psychosis can be challenging to differentiate from other mental disorders with similar symptoms, such as:
- Schizophrenia: While IOR psychosis shares some symptoms with schizophrenia, it typically lacks the disorganized thinking, hallucinations, and social withdrawal characteristic of schizophrenia.
- Mood disorders: Depressive or manic episodes can sometimes involve delusions, but these delusions are typically congruent with the individual’s mood and resolve with the resolution of the episode.
- Obsessive-compulsive disorder: Obsessions can be similar to IOR beliefs, but they are typically more specific, repetitive, and accompanied by anxiety or distress.
Treatment Approaches
The treatment of IOR psychosis typically involves a combination of medication and psychotherapy.
- Medication: Antipsychotic medications, such as risperidone and olanzapine, can help to reduce the severity of delusions and improve overall functioning.
- Psychotherapy: Cognitive-behavioral therapy (CBT) is an effective psychotherapy for IOR psychosis. CBT focuses on challenging the individual’s irrational beliefs and developing coping mechanisms to manage the symptoms of the disorder.
Emerging Concepts
Recent research has highlighted the importance of considering the following emerging concepts in the understanding and treatment of IOR psychosis:
- Personalization: IOR beliefs may be influenced by the individual’s personality traits, particularly those related to egocentricity and self-importance.
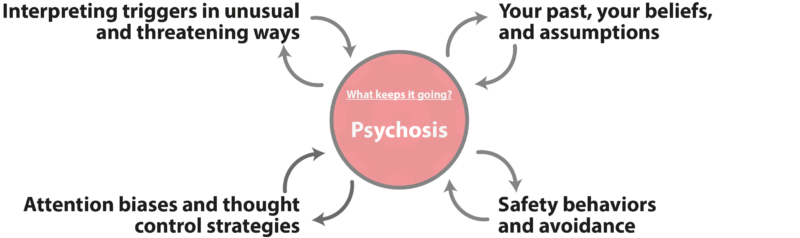
- Cognitive biases: Individuals with IOR psychosis may exhibit cognitive biases, such as attentional biases towards personally relevant stimuli and confirmation bias.
- Social factors: Social isolation and lack of social support can contribute to the development and maintenance of IOR beliefs.
Future Directions
Future research on IOR psychosis will likely focus on the following areas:
- Neurobiological markers: Identifying neurobiological markers that can aid in diagnosis and predict treatment response.
- Personalized treatment: Developing personalized treatment plans based on the individual’s unique clinical presentation and underlying mechanisms.
- Technology-based interventions: Exploring the use of virtual reality and other technology-based interventions to improve treatment outcomes.
Conclusion
Ideas of reference psychosis is a complex and challenging mental disorder that requires a comprehensive approach to treatment. Advances in neuroscience and psychology have provided valuable insights into the underlying mechanisms and treatment options for this condition. As research continues to progress, we can expect to see further advancements in diagnosis, treatment, and support for individuals with IOR psychosis.
![[IMGSRCTITLE2]](https://m.media-amazon.com/images/I/71EXPmuSj+L._SL1500_.jpg)
![[IMGSRCTITLE3]](https://img.meepshop.com/D0yhbJCQ36ve0YrDDOkcupqQJI2ISOjF2Ds0CZBY_j0/w:480/Z3M6Ly9pbWcubWVlcGNsb3VkLmNvbS9tZWVwc2hvcC9iYjgyNzE0NS04ODViLTQzYjktYTVhMC1lNTU2NjdlYWRlNDAvZmlsZXMvMDc0M2M1NjEtNjMwNi00N2U4LWJmMmItOTc0OGZjODMzMjYyLmpwZWc)
![[IMGSRCTITLE4]](https://brainary-cdn.s3.ap-southeast-2.amazonaws.com/app/uploads/2022/04/24221747/9781583917237.jpg)
![[IMGTITLE5]](https://www.wasatch.org/blog/wp-content/uploads/2023/01/What-is-Psychosis.png)
![[IMGTITLE6]](https://mind.help/wp-content/uploads/2021/07/What-is-Psychosis-1.webp)
![[IMGTITLE7]](https://i1.rgstatic.net/publication/287660081_Evolving_Psychosis_Different_Stages_Different_Treatmentsedited_by_Jan_Olav_Johannessen_Brian_V_Martindale_and_Johan_Cullberg_New_York_Routledge_2006_298_pages_3595_softcover/links/56a29dad08aeef24c585f9a8/largepreview.png)
![[IMGTITLE8]](https://image.slidesharecdn.com/read-book-psychosis-trauma-and-dissociation-evolving-perspectives-on-severe-psychopathology-free-210105102844/95/read-book-psychosis-trauma-and-dissociation-evolving-perspectives-on-severe-psychopathology-free-7-638.jpg?cb=1609842538)
![[IMGTITLE9]](https://s3.amazonaws.com/utep-uploads/wp-content/uploads/online-regis-college/2023/04/20024602/IG01.jpg)
Closure
Thus, we hope this article has provided valuable insights into Ideas of Reference Psychosis in 2025: An Exploration of Evolving Concepts and Treatment Approaches. We appreciate your attention to our article. See you in our next article!